Understanding Degenerative Disc Disease
Degenerative disc disease (DDD) affects millions of people worldwide, causing chronic back pain and limiting daily activities. While the term “cure” might be misleading since DDD is a natural aging process, many patients have successfully managed their symptoms and achieved pain-free lives through comprehensive treatment approaches.
This article explores evidence-based treatment methods, personal recovery stories, and the latest medical advances in treating degenerative disc disease, providing readers with actionable insights for their own healing journey. Similar to how patients manage chronic knee conditions, degenerative disc disease requires a comprehensive, long-term approach to achieve optimal outcomes.
How to cure degenerative disc disease (DDD) in a few minutes!
What is Degenerative Disc Disease?
Table 1: DDD vs Normal Disc Characteristics
| Aspect | Healthy Disc | Degenerative Disc |
|---|---|---|
| Water Content | 80-85% | 60-70% |
| Height | Normal spacing | Reduced height |
| Flexibility | High mobility | Limited movement |
| Shock Absorption | Excellent | Compromised |
| Pain Level | None | Mild to severe |
Degenerative disc disease isn’t technically a disease but rather describes the natural wear and tear that occurs in spinal discs over time. The intervertebral discs act as cushions between vertebrae, providing flexibility and shock absorption to the spine.
Key Characteristics of DDD:
- Loss of disc height and water content
- Development of bone spurs (osteophytes)
- Inflammation around affected areas
- Reduced spinal mobility
- Chronic pain patterns
Personal Success Stories: How Patients Overcame DDD
Case Study 1: Sarah’s Journey to Recovery
Sarah, a 45-year-old office worker, experienced severe lower back pain for three years before finding relief through a combination of physical therapy, lifestyle modifications, and regenerative treatments. Her recovery timeline demonstrates the importance of consistent, multi-modal treatment approaches, much like the comprehensive care required for other musculoskeletal conditions.
Treatment Timeline:
- Months 1-3: Physical therapy foundation building
- Months 4-6: Advanced exercise protocols
- Months 7-9: Lifestyle optimization
- Months 10-12: Maintenance and prevention
Case Study 2: Michael’s Athletic Recovery
A former athlete in his 50s, Michael combined traditional treatments with cutting-edge regenerative medicine to return to competitive sports within 18 months.
Evidence-Based Treatment Options
Table 2: Treatment Effectiveness Comparison
| Treatment Method | Success Rate | Recovery Time | Cost Range | Side Effects |
|---|---|---|---|---|
| Physical Therapy | 70-85% | 3-6 months | $500-2000 | Minimal |
| Medication | 60-75% | 2-8 weeks | $50-500/month | Moderate |
| Injections | 65-80% | 1-3 months | $1000-3000 | Low-Moderate |
| Surgery | 80-90% | 6-12 months | $20,000-100,000 | High |
| Regenerative Medicine | 70-85% | 3-12 months | $3000-15,000 | Minimal |
Non-Surgical Treatment Approaches
1. Physical Therapy and Exercise
Physical therapy remains the cornerstone of DDD treatment, focusing on:
Core Strengthening Exercises:
- Plank variations
- Dead bug exercises
- Bird dog poses
- Pelvic tilts
Learn more about comprehensive fitness approaches that can support your recovery journey.
Flexibility and Mobility Work:
- Cat-cow stretches
- Knee-to-chest stretches
- Piriformis stretches
- Hip flexor stretches
Table 3: Exercise Protocol Progression
| Week | Core Exercises | Duration | Frequency | Intensity |
|---|---|---|---|---|
| 1-2 | Basic planks | 15-30 sec | 3x/week | Low |
| 3-4 | Modified planks | 30-45 sec | 4x/week | Low-Medium |
| 5-8 | Advanced planks | 45-60 sec | 5x/week | Medium |
| 9-12 | Dynamic planks | 60+ sec | 5x/week | Medium-High |
2. Pain Management Strategies
Medication Options:
- NSAIDs (Ibuprofen, Naproxen)
- Muscle relaxants
- Nerve pain medications (Gabapentin, Pregabalin)
- Topical analgesics
Alternative Pain Management:
- Acupuncture
- Massage therapy
- Heat/cold therapy
- TENS units
For those dealing with chronic pain-related mental health challenges, it’s important to address both physical and psychological aspects of recovery.
3. Lifestyle Modifications
Table 4: Lifestyle Factors Impact on DDD
| Factor | Positive Impact | Negative Impact | Recommendation |
|---|---|---|---|
| Weight Management | Reduces spinal load | Increases pressure | Maintain BMI <25 |
| Smoking | None | Reduces disc nutrition | Complete cessation |
| Sleep Position | Proper alignment | Poor posture | Side sleeping with pillow |
| Ergonomics | Reduces strain | Increases stress | Proper workstation setup |
| Nutrition | Anti-inflammatory | Pro-inflammatory | Mediterranean diet |
Image Placement 6: [Ergonomic workspace setup diagram – Alt text: “Proper ergonomic desk setup for degenerative disc disease prevention”]
Advanced Treatment Options
Regenerative Medicine Approaches
Stem Cell Therapy
Recent clinical trials show promising results for stem cell treatments in DDD management. According to Mayo Clinic research, the therapy involves:
- Harvesting mesenchymal stem cells
- Processing and concentration
- Direct injection into affected discs
- Monitoring regeneration over 6-12 months
Table 5: Regenerative Treatment Comparison
| Treatment Type | Mechanism | Success Rate | Duration | Cost |
|---|---|---|---|---|
| Stem Cell Therapy | Disc regeneration | 75-85% | 6-12 months | $5,000-15,000 |
| PRP Injections | Growth factor stimulation | 65-75% | 3-6 months | $1,500-3,000 |
| Injectable Gels | Disc volume restoration | 70-80% | 6-9 months | $3,000-8,000 |
Platelet-Rich Plasma (PRP)
PRP therapy utilizes the patient’s own platelets to promote healing and reduce inflammation in affected discs. Research from the American Journal of Sports Medicine demonstrates significant pain reduction in 65-75% of patients treated with PRP injections.
Surgical Interventions
When Surgery May Be Necessary:
- Conservative treatment failure after 6+ months
- Progressive neurological symptoms
- Severe functional impairment
- Cauda equina syndrome
Surgical Options:
- Discectomy – Removal of herniated disc material
- Spinal Fusion – Joining adjacent vertebrae
- Artificial Disc Replacement – Mechanical disc substitution
- Minimally Invasive Procedures – Endoscopic techniques
Prevention and Long-term Management
Table 6: Prevention Strategies Effectiveness
| Strategy | Effectiveness | Implementation Difficulty | Long-term Benefits |
|---|---|---|---|
| Regular Exercise | High | Medium | Excellent |
| Weight Management | High | High | Excellent |
| Proper Ergonomics | Medium | Low | Good |
| Stress Management | Medium | Medium | Good |
| Smoking Cessation | High | High | Excellent |
Daily Management Strategies
Morning Routine
- Gentle stretching exercises
- Proper posture awareness
- Anti-inflammatory breakfast
- Ergonomic workspace setup
Throughout the Day
- Regular movement breaks
- Proper lifting techniques
- Stress management practices
- Hydration maintenance
Evening Routine
- Relaxation exercises
- Heat therapy
- Sleep position optimization
- Reflection and planning
Nutritional Approaches to DDD Management
Table 7: Anti-Inflammatory Foods vs Pro-Inflammatory Foods
| Anti-Inflammatory | Pro-Inflammatory |
|---|---|
| Fatty fish (salmon, mackerel) | Processed meats |
| Leafy greens (spinach, kale) | Refined sugars |
| Berries (blueberries, cherries) | Trans fats |
| Nuts and seeds | Excessive alcohol |
| Olive oil | Processed foods |
| Turmeric and ginger | High-sodium foods |
Supplements for DDD Support
Evidence-Based Supplements:
- Glucosamine/Chondroitin: Joint cartilage support
- Omega-3 fatty acids: Inflammation reduction according to Harvard Health
- Vitamin D: Bone health maintenance as recommended by National Institutes of Health
- Magnesium: Muscle relaxation
- Turmeric (Curcumin): Natural anti-inflammatory properties documented by Johns Hopkins Medicine
Technology and Innovation in DDD Treatment
Emerging Technologies
Artificial Intelligence in Diagnosis
AI-powered imaging analysis provides:
- Earlier detection of disc degeneration
- Personalized treatment recommendations
- Progress monitoring capabilities
- Predictive outcome modeling
Bioengineering Solutions
- 3D-printed disc implants
- Biocompatible gel injections
- Nanotechnology drug delivery
- Gene therapy applications
Table 8: Technology Timeline and Availability
| Technology | Current Status | Expected Availability | Potential Impact |
|---|---|---|---|
| AI Diagnosis | Available | Currently | High |
| Injectable Gels | Clinical Trials | 2025-2026 | High |
| Gene Therapy | Research Phase | 2027-2030 | Very High |
| 3D Printed Discs | Development | 2026-2028 | Very High |
Mental Health and DDD Recovery
Psychological Impact of Chronic Pain
Degenerative disc disease often affects mental health through:
- Chronic pain stress
- Activity limitations
- Sleep disturbances
- Social isolation
- Depression and anxiety
Just as with other chronic conditions, addressing the psychological component is crucial for recovery. Our guide on managing anxiety provides additional strategies for mental health support during physical recovery.
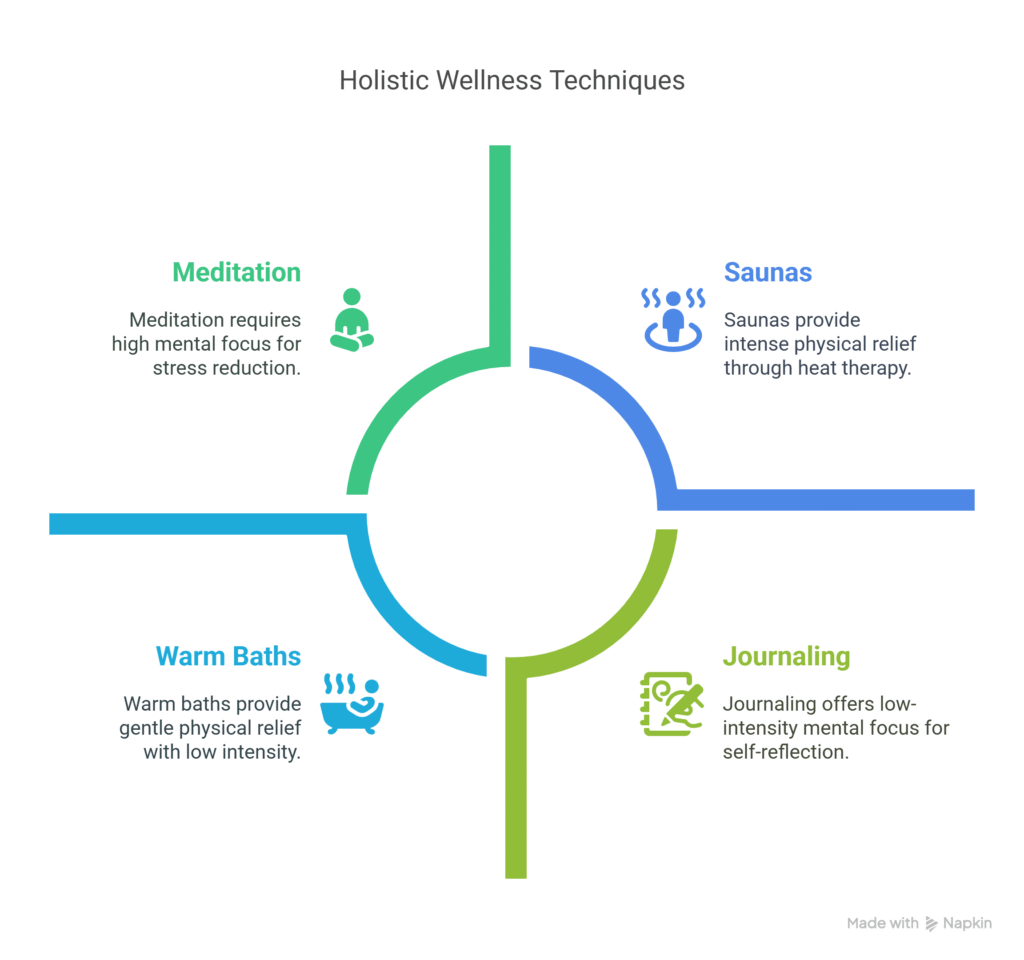
Coping Strategies
Table 9: Mental Health Support Options
| Approach | Effectiveness | Accessibility | Cost |
|---|---|---|---|
| Cognitive Behavioral Therapy | High | Medium | $100-200/session |
| Mindfulness Meditation | Medium-High | High | Free-$50/month |
| Support Groups | Medium | High | Free-$25/session |
| Stress Reduction Programs | Medium | Medium | $200-500/program |
Creating Your Personal Recovery Plan
Step-by-Step Recovery Framework
Phase 1: Assessment and Foundation (Weeks 1-4)
- Medical Evaluation
- Comprehensive imaging studies
- Pain assessment scores
- Functional capacity evaluation
- Baseline measurements
- Team Assembly
- Primary care physician
- Orthopedic or neurosurgical specialist
- Physical therapist
- Pain management specialist (if needed)
Phase 2: Active Treatment (Weeks 5-16)
- Physical Therapy Protocol
- 3x weekly sessions initially
- Home exercise program
- Progress monitoring
- Activity modification
- Pain Management
- Medication optimization
- Alternative therapies
- Lifestyle modifications
- Stress management
Phase 3: Optimization and Maintenance (Weeks 17-52)
- Advanced Interventions (if needed)
- Injection therapies
- Regenerative treatments
- Surgical consultation
- Long-term Strategies
- Exercise maintenance
- Prevention protocols
- Regular monitoring
- Lifestyle sustainability
Table 10: Recovery Milestones Timeline
| Timeframe | Expected Outcomes | Key Indicators |
|---|---|---|
| 4 weeks | Pain reduction 20-30% | Improved daily function |
| 8 weeks | Pain reduction 40-50% | Return to light activities |
| 12 weeks | Pain reduction 60-70% | Improved sleep quality |
| 24 weeks | Pain reduction 70-80% | Return to most activities |
| 52 weeks | Maintenance achieved | Long-term stability |
Cost Analysis and Insurance Considerations
Table 11: Treatment Cost Analysis
| Treatment Category | Initial Cost | Annual Cost | Insurance Coverage |
|---|---|---|---|
| Conservative Care | $500-2,000 | $1,000-3,000 | 80-100% |
| Advanced Injections | $1,000-5,000 | $2,000-8,000 | 60-80% |
| Regenerative Medicine | $3,000-15,000 | $1,000-5,000 | 0-40% |
| Surgical Intervention | $20,000-100,000 | $2,000-10,000 | 70-90% |
Insurance Navigation Tips
- Prior Authorization – Ensure all treatments are pre-approved
- Documentation – Maintain detailed medical records
- Appeals Process – Understand denial procedures
- Network Providers – Use in-network specialists when possible
Research and Future Directions
Current Clinical Trials
Recent studies focus on:
- Novel biomaterials for disc replacement
- Gene therapy for disc regeneration according to Nature Medicine
- Advanced stem cell techniques
- Minimally invasive surgical approaches developed by Cleveland Clinic
Promising Research Areas
Table 12: Research Pipeline Overview
| Research Area | Development Stage | Timeline | Potential Impact |
|---|---|---|---|
| Biomaterial Implants | Phase II Trials | 2-3 years | High |
| Gene Therapy | Preclinical | 5-7 years | Very High |
| AI-Guided Surgery | Early Clinical | 1-2 years | Medium-High |
| Personalized Medicine | Development | 3-5 years | High |
Frequently Asked Questions
Common Patient Concerns
Q: Can degenerative disc disease be completely cured? A: While DDD represents natural aging changes that cannot be completely reversed, many patients achieve complete pain relief and return to normal activities through comprehensive treatment approaches. According to Spine Journal research, 70-85% of patients experience significant improvement with proper treatment.
Q: How long does recovery typically take? A: Recovery timelines vary significantly based on severity, treatment approach, and individual factors. Most patients see significant improvement within 3-6 months of consistent treatment, similar to recovery patterns observed in other musculoskeletal conditions.
Q: Are there any activities I should permanently avoid? A: While most activities can be resumed with proper conditioning, high-impact sports and heavy lifting may require permanent modifications or specialized techniques.
Q: What’s the success rate of different treatments? A: Success rates vary by treatment type and individual factors, ranging from 60-90% depending on the approach and severity of the condition. The American Academy of Orthopaedic Surgeons reports that conservative treatments show success rates of 80-90% when properly implemented.
Conclusion: Your Path to Recovery
Degenerative disc disease management requires a comprehensive, personalized approach combining evidence-based treatments with lifestyle modifications. While the journey to recovery can be challenging, the success stories and advancing treatment options provide hope for millions suffering from this condition.
For additional health resources and related conditions, explore our comprehensive guides on oral health and managing chronic conditions.
The key to successful DDD management lies in:
- Early intervention and proper diagnosis
- Comprehensive treatment planning
- Consistent adherence to therapy protocols
- Long-term lifestyle modifications
- Regular monitoring and adjustment
Remember that recovery is a process, not a destination. With proper guidance, dedication, and the right treatment approach, most individuals can achieve significant pain relief and return to their desired quality of life.
Final Recommendations
- Consult with specialists early in your journey
- Commit to conservative treatments for at least 3-6 months
- Consider advanced options if conservative care fails
- Focus on prevention and long-term maintenance
- Stay informed about emerging treatments and research
Table 13: Action Steps Summary
| Priority | Action Item | Timeline | Resources Needed |
|---|---|---|---|
| High | Medical evaluation | Week 1 | Healthcare provider |
| High | Begin physical therapy | Week 2-3 | PT referral |
| Medium | Lifestyle modifications | Weeks 1-4 | Personal commitment |
| Medium | Pain management plan | Weeks 2-4 | Medical guidance |
| Low | Consider advanced treatments | Months 3-6 | Specialist consultation |
Your journey to recovery from degenerative disc disease is unique, but you’re not alone. With the right information, support, and treatment approach, a pain-free future is achievable.

![Comparative MRI images showing healthy vs degenerative discs - Alt text: "MRI comparison healthy spine versus degenerative disc disease"]](http://discoverbribune.site/wp-content/uploads/2025/06/Comparative-MRI-images-showing-healthy-vs-degenerative-discs-Alt-text_-_MRI-comparison-healthy-spine-versus-degenerative-disc-disease_-1024x579.webp)


![Exercise demonstration photos showing proper form - Alt text: "Physical therapy exercises for degenerative disc disease demonstration"]](http://discoverbribune.site/wp-content/uploads/2025/06/Exercise-demonstration-photos-showing-proper-form-Alt-text_-_Physical-therapy-exercises-for-degenerative-disc-disease-demonstration_-1024x579.webp)
![Medical procedure illustration of stem cell injection - Alt text: "Stem cell therapy procedure for degenerative disc disease treatment"]](http://discoverbribune.site/wp-content/uploads/2025/06/Medical-procedure-illustration-of-stem-cell-injection-Alt-text_-_Stem-cell-therapy-procedure-for-degenerative-disc-disease-treatment_-1024x579.webp)
![Surgical procedure comparison diagram - Alt text: "Comparison of surgical procedures for degenerative disc disease"]](http://discoverbribune.site/wp-content/uploads/2025/06/Surgical-procedure-comparison-diagram-Alt-text_-_Comparison-of-surgical-procedures-for-degenerative-disc-disease_-1024x579.webp)
![[Lifestyle modification infographic - Alt text: "Degenerative disc disease prevention lifestyle modifications infographic"]](http://discoverbribune.site/wp-content/uploads/2025/06/Lifestyle-modification-infographic-Alt-text_-_Degenerative-disc-disease-prevention-lifestyle-modifications-infographic_-1024x579.jpg)

![Anti-inflammatory foods arrangement photo - Alt text: "Anti-inflammatory foods for degenerative disc disease management"]](http://discoverbribune.site/wp-content/uploads/2025/06/Anti-inflammatory-foods-arrangement-photo-Alt-text_-_Anti-inflammatory-foods-for-degenerative-disc-disease-management_-1024x579.webp)

![Meditation/mindfulness practice photo - Alt text: "Mental health support for degenerative disc disease recovery"]](http://discoverbribune.site/wp-content/uploads/2025/06/Meditation_mindfulness-practice-photo-Alt-text_-_Mental-health-support-for-degenerative-disc-disease-recovery_-1024x579.webp)
![[Healthcare cost comparison chart - Alt text: "Healthcare costs comparison for degenerative disc disease treatments"]](http://discoverbribune.site/wp-content/uploads/2025/06/Healthcare-cost-comparison-chart-Alt-text_-_Healthcare-costs-comparison-for-degenerative-disc-disease-treatments_-1024x579.webp)

![Success/recovery celebration photo - Alt text: "Successful degenerative disc disease recovery celebration"]](http://discoverbribune.site/wp-content/uploads/2025/06/Success_recovery-celebration-photo-Alt-text_-_Successful-degenerative-disc-disease-recovery-celebration_-1024x579.webp)