Osgood-Schlatter disease in adults represents a continuation or recurrence of a condition that typically develops during adolescence. While most commonly associated with growing children and teenagers, this condition can persist into adulthood or develop as a residual problem from untreated adolescent cases.
What is Osgood-Schlatter Disease?
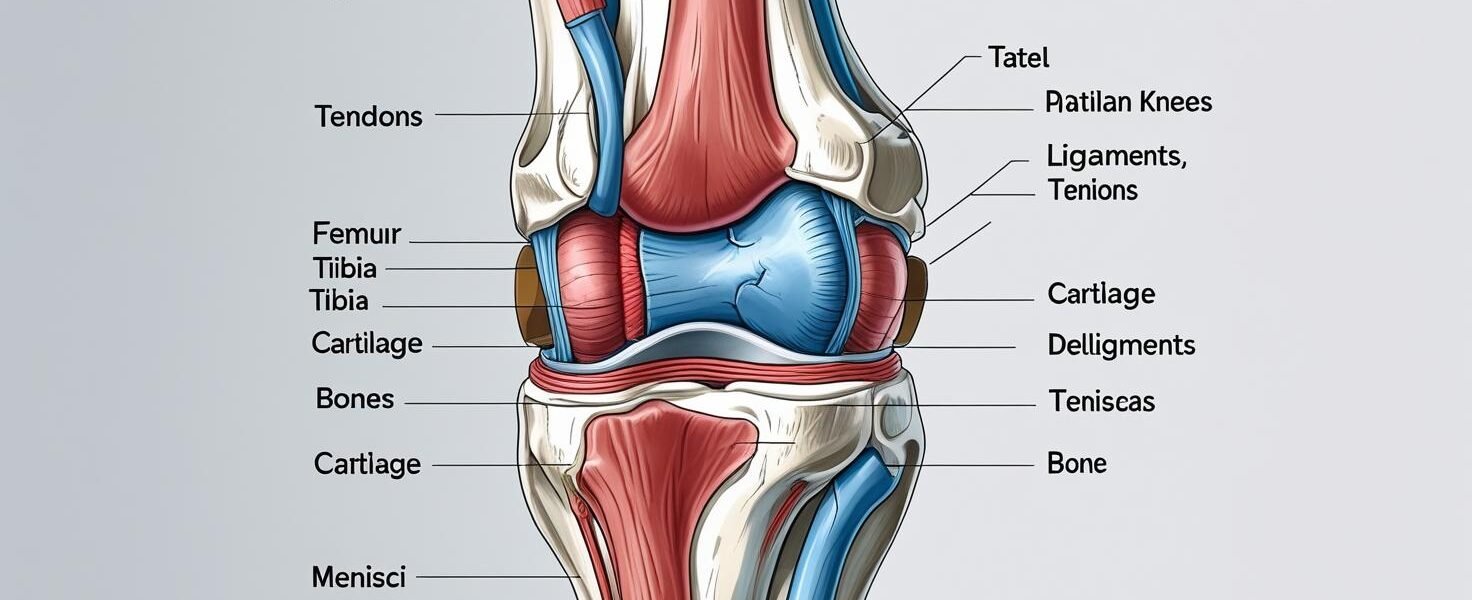
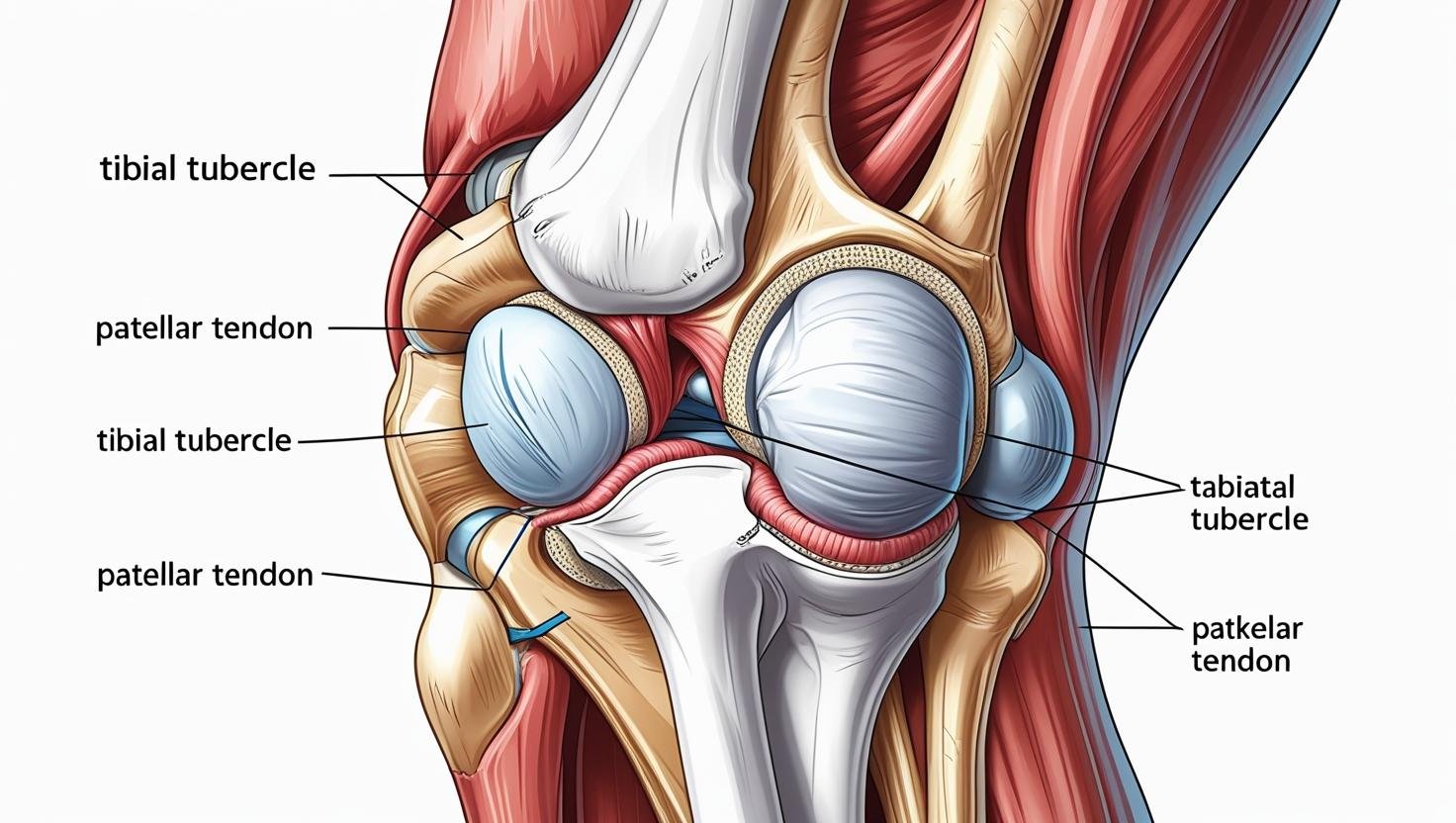
Osgood-Schlatter disease is a painful condition affecting the area just below the kneecap, specifically at the tibial tubercle where the patellar tendon attaches to the shinbone. In adults, this condition manifests as chronic anterior knee pain and can significantly impact daily activities and athletic performance.
Historical Background
The condition was first described simultaneously in 1903 by two physicians: Robert Osgood (1873-1956), a US orthopedic surgeon, and Carl Schlatter (1864-1934), a Swiss surgeon, giving the disease its current name.
Adult vs. Adolescent Presentation
| Aspect | Adolescent Presentation | Adult Presentation |
|---|---|---|
| Age Range | 9-15 years | 18+ years |
| Primary Cause | Growth plate irritation | Residual symptoms, overuse |
| Pain Pattern | Activity-related, intermittent | Chronic, persistent |
| Recovery Time | Weeks to months | Months to years |
| Treatment Response | Usually excellent | More challenging |
| Long-term Outlook | Generally resolves | May require ongoing management |
Symptoms and Clinical Presentation
Primary Symptoms
Adult patients with Osgood-Schlatter disease typically experience:
- Anterior Knee Pain
- Dull in nature and localized to the area of injury
- Located directly over the tibial tubercle
- Worsens with physical activity, especially running and jumping
- Swelling and Inflammation
- Swelling and anterior knee pain are most commonly associated with Osgood Schlatter disease
- Visible enlargement of the tibial tubercle
- Tenderness to touch
- Functional Limitations
- Difficulty with stairs (especially descending)
- Pain during squatting or kneeling
- Reduced athletic performance
Secondary Symptoms
| Symptom | Frequency in Adults | Severity Rating (1-10) |
|---|---|---|
| Tibial tubercle pain | 95% | 6-8 |
| Swelling | 80% | 4-6 |
| Activity limitation | 85% | 5-7 |
| Night pain | 25% | 3-5 |
| Knee stiffness | 60% | 4-6 |
Diagnostic Criteria
Healthcare providers assess adult Osgood-Schlatter disease based on:
- Patient history of adolescent knee problems
- Physical examination findings
- Imaging studies (X-rays, MRI)
- Response to conservative treatment
Causes and Risk Factors
Primary Causes in Adults
- Residual Adolescent Condition
- Incomplete healing during teenage years
- Persistent bony prominence at tibial tubercle
- Chronic inflammation from previous injury
- Overuse and Repetitive Stress
- High-impact sports participation
- Sudden increase in training intensity
- Poor biomechanics during activities
- Anatomical Factors
- Prominent tibial tubercle
- Tight quadriceps muscles
- Poor flexibility
Risk Factors
| Risk Factor | Impact Level | Modifiable |
|---|---|---|
| Previous adolescent OSD | High | No |
| High-impact sports | High | Yes |
| Poor flexibility | Medium | Yes |
| Muscle imbalances | Medium | Yes |
| Overtraining | High | Yes |
| Age (18-25) | Medium | No |
| Gender (slight male predominance) | Low | No |
Sports Most Commonly Associated
- Basketball
- Soccer
- Running (especially sprinting)
- Volleyball
- Tennis
- Gymnastics
Diagnosis and Assessment
Clinical Examination
Healthcare providers use several assessment techniques:
- Physical Examination
- The enlarged, inflamed tibial tubercle is nearly always tender when pressure is applied
- Palpation of the tibial tubercle
- Range of motion testing
- Muscle strength assessment
- Imaging Studies
- X-rays: Show bony prominence and fragmentation
- MRI: Reveals soft tissue inflammation
- Ultrasound: Assesses tendon integrity
Differential Diagnosis
| Condition | Key Differentiating Features |
|---|---|
| Patellar tendinitis | Pain at patellar tendon, not tibial tubercle |
| Patellofemoral pain syndrome | Retropatellar pain, different pain pattern |
| Tibial stress fracture | Different location, specific imaging findings |
| Bursitis | Fluid collection, different pain characteristics |
Diagnostic Criteria
For adult diagnosis, patients typically present with:
- History of adolescent knee problems
- Persistent anterior knee pain
- Tenderness over tibial tubercle
- Imaging confirmation of bony changes
Treatment Options
Conservative Management
The foundation of treatment involves non-surgical approaches:
- Activity Modification
- Limiting activities that cause pain, reducing time spent running, jumping, or participating in sports until symptoms improve
- Gradual return to activity
- Cross-training with low-impact exercises
- Pain Management
- Symptomatic treatment with ice and NSAIDs
- Applying ice to the affected area can help reduce pain and swelling
- Anti-inflammatory medications
- Physical Therapy
- Stretching programs for quadriceps and hamstrings
- Strengthening exercises
- Biomechanical correction
Treatment Modalities Comparison
| Treatment | Effectiveness | Time to Improvement | Cost |
|---|---|---|---|
| Rest and ice | Moderate | 2-4 weeks | Low |
| Physical therapy | High | 4-8 weeks | Medium |
| Anti-inflammatories | Moderate | 1-2 weeks | Low |
| Bracing/strapping | Moderate | Immediate | Low |
| Injection therapy | High | 1-2 weeks | Medium |
| Surgery | Very High | 3-6 months | High |
Advanced Treatment Options
- Injection Therapy
- Corticosteroid injections
- Platelet-rich plasma (PRP)
- Hyaluronic acid
- Surgical Intervention
- Reserved for severe, persistent cases
- Removal of loose bone fragments
- Tendon repair or reconstruction
Treatment Protocol by Severity
| Severity Level | Symptoms | Recommended Treatment |
|---|---|---|
| Mild | Occasional pain, minimal swelling | Rest, ice, NSAIDs |
| Moderate | Regular pain, activity limitation | PT, bracing, activity modification |
| Severe | Constant pain, significant limitation | Injection therapy, consider surgery |
Long-term Complications
Potential Complications
Adult Osgood-Schlatter disease can lead to several long-term issues:
- Chronic Pain Syndrome
- Persistent anterior knee pain
- Activity-related discomfort
- Reduced quality of life
- Functional Limitations
- Difficulty with high-impact activities
- Occupational limitations
- Reduced athletic performance
- Structural Changes
- Permanent bony prominence
- Altered knee biomechanics
- Compensatory movement patterns
Long-term Prognosis
Research indicates that long-term prognosis evaluation 2 to 6 years after diagnosis shows varying outcomes, with some patients experiencing complete resolution while others develop chronic symptoms.
| Outcome | Percentage of Patients | Timeframe |
|---|---|---|
| Complete resolution | 60-70% | 1-2 years |
| Mild residual symptoms | 20-25% | Ongoing |
| Moderate limitations | 10-15% | Ongoing |
| Severe chronic pain | 5% | Ongoing |
Prevention Strategies
Primary Prevention
- Proper Training Techniques
- Gradual activity progression
- Adequate warm-up and cool-down
- Sport-specific conditioning
- Flexibility Maintenance
- Regular quadriceps stretching
- Hamstring flexibility exercises
- Hip flexor stretching
- Strength Training
- Balanced quadriceps and hamstring strength
- Core stability exercises
- Proper biomechanics training
Secondary Prevention
| Risk Level | Prevention Strategy | Frequency |
|---|---|---|
| Low risk | General fitness, flexibility | 3x/week |
| Moderate risk | Targeted exercises, monitoring | 5x/week |
| High risk | Comprehensive program, professional guidance | Daily |
Personal Review and Patient Experiences
Case Study 1: Recreational Athlete
Sarah, a 28-year-old weekend warrior, experienced recurrent knee pain during basketball games. Her adolescent Osgood-Schlatter disease had seemingly resolved, but symptoms returned with increased athletic activity. Through a combination of physical therapy, activity modification, and proper conditioning, she successfully managed her symptoms and returned to competitive play within 12 weeks.
Case Study 2: Former Elite Athlete
Michael, a 35-year-old former college soccer player, dealt with chronic anterior knee pain that limited his coaching activities. His condition required a multidisciplinary approach including injection therapy and surgical intervention to remove loose bone fragments. Post-surgery, he experienced significant improvement and was able to resume active coaching.
Patient Testimonials
“The key to managing my adult Osgood-Schlatter disease was understanding that it’s a chronic condition that requires ongoing management. Physical therapy and proper training techniques have been game-changers for me.” – Former patient, age 32
Treatment Success Factors
| Factor | Impact on Success | Patient Control |
|---|---|---|
| Early intervention | High | High |
| Compliance with treatment | Very High | High |
| Activity modification | High | High |
| Professional guidance | High | Medium |
| Patient education | Medium | High |
Frequently Asked Questions
Q1: Can Osgood-Schlatter disease develop for the first time in adults?
A: While rare, Osgood-Schlatter disease can affect adults if not properly assessed and treated. Most adult cases represent continuation of adolescent conditions or development of symptoms due to overuse.
Q2: How long does treatment typically take in adults?
A: Treatment duration varies significantly, ranging from 6 weeks for mild cases to 6-12 months for severe cases requiring comprehensive management.
Q3: Is surgery always necessary for adult Osgood-Schlatter disease?
A: No, surgery is rarely used to treat Osgood-Schlatter disease. Most cases respond well to conservative treatment including activity modification, physical therapy, and pain management.
Q4: Can adults return to high-impact sports after treatment?
A: Many adults can return to sports activities, though this may require ongoing management, proper conditioning, and sometimes activity modification to prevent symptom recurrence.
Q5: What’s the difference between adult and adolescent Osgood-Schlatter disease?
A: Adult cases typically involve chronic symptoms, take longer to resolve, and may require more intensive treatment compared to adolescent cases that usually resolve with skeletal maturity.
| Question Topic | Key Point | Treatment Implication |
|---|---|---|
| Adult onset | Possible but uncommon | Requires thorough evaluation |
| Treatment duration | 6 weeks to 12 months | Patience and compliance crucial |
| Surgery necessity | Rarely required | Conservative approach preferred |
| Sports return | Often possible | May need modifications |
| Adult vs. adolescent | More chronic in adults | Requires long-term management |
Conclusion
Osgood-Schlatter disease in adults represents a challenging condition that requires comprehensive understanding and management. While the condition can significantly impact quality of life and athletic performance, proper diagnosis and treatment can lead to successful outcomes in the majority of cases. The key to successful management lies in early intervention, patient education, and a multidisciplinary approach that addresses both the physical and functional aspects of the condition.
Healthcare providers should maintain a high index of suspicion for adult Osgood-Schlatter disease in patients presenting with anterior knee pain, particularly those with a history of adolescent knee problems or participation in high-impact sports. With appropriate treatment and ongoing management, most adults can achieve significant symptom relief and return to desired activity levels.


![X-ray image showing characteristic bony prominence of tibial tubercle]](http://discoverbribune.site/wp-content/uploads/2025/06/X-ray-image-showing-characteristic-bony-prominence-of-tibial-tubercle-1.webp)